The most common clinical form of MS presents with a relapsing-remitting course (RRMS). Several immune parameters are different between RRMS patients and healthy subjects, such as imbalance of pro- vs. anti-inflammatory cytokines, chemokine receptor and adhesion molecule changes and deficient CD4 and CD8 Treg function, among others. Most of these observations have been made during the quiescent stage of disease, partly due to the inherent difficulty in recruiting patients during an acute relapse but before the administration of steroid therapy. Thus, the immunologic basis of a clinical relapse remains poorly understood.
Whereas some studies have shown aberrant immune responses to myelin antigens and defective T- and B-regs, the immune dysregulation that underlies the relapse remains unclear. In particular, there is a paucity of longitudinal studies addressing CD4 and CD8 T cell effector and regulatory responses before, during and after an acute relapse. Through collaborative efforts at two institutions, we have been able to put in place a streamlined recruitment mechanism, whereby patients presenting with an acute relapse [both treatment-naïve as well as those on some therapy] can be studied before any steroids are administered. Our studies thus far have focused on treatment-naïve RRMS patients in acute relapse. Using innovative approaches, we have made several novel observations regarding Immune regulatory biology during acute MS relapse:
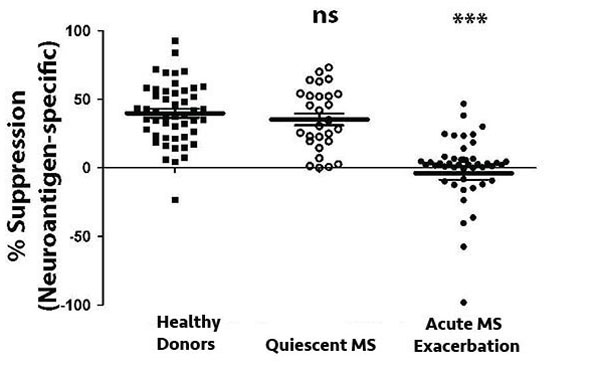
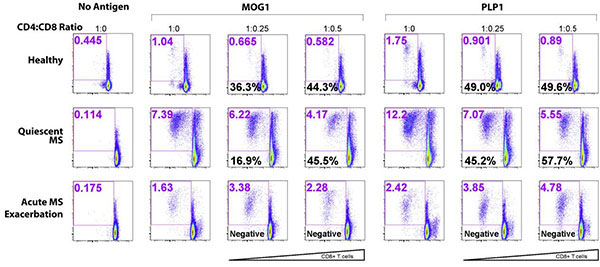
- We demonstrated the novel and unexpected immune regulatory function of CNS-specific CD8+ T cells. Interestingly, RRMS patients with quiescent disease and healthy subjects showed comparable levels of CNS-specific CD8 suppressor activity. However, patients during an acute relapse showed a dramatic deficit of CNS-specific suppressor activity.
- As patients attained disease quiescence (with various different therapies), they consistently showed normalization of CNS-specific CD8 suppressor activity.
- The suppressive activity of these cells was HLA-Class I restricted and dependent on IFN-γ as well as perforin and granzyme B expression, involving cytolytic activity on CD4 T cells and APC populations.
- Interestingly, CNS-specific CD8 regulatory activity was harbored in the terminally differentiated subset of CD8 T cells. Importantly, this subset was deficient during an acute relapse of MS.
- The suppressor activity of relapse-associated CD8 T cells could be restored by in vitro pre-treatment with specific cytokines, such as IL-12, revealing potentially novel therapeutic approaches.
- Finally, in addition to a deficit of CD8-instrinsic regulatory function, we also observed a relative resistance of CD4 effector T cells to suppression during an acute relapse.
Based on these preliminary findings, we hypothesize that a clinical relapse of MS is caused by an accumulating longitudinal deficit of CD8 regulatory function and increasing CD4 resistance. We further hypothesize that this regulatory deficit is the result of a blockade in terminal differentiation of CNS-specific CD8 T cells. As a corollary, we propose that correcting these functional deficits is an important immunologic correlate of disease quiescence.
We are addressing these central hypotheses through ongoing experiments, with longitudinal immunologic monitoring of patients through their course of treatment and their recovery from relapses. Simultaneously, we are dissecting the mechanisms of regulatory deficit and effector resistance seen during disease relapse.
Learn More:
Neuroantigen-specific CD8+ regulatory T-cell function is deficient during acute exacerbation of multiple sclerosis. Baughman EJ, Mendoza JP, Ortega SB, Ayers CL, Greenberg BM, Frohman EM, Karandikar NJ. J Autoimmun. 2011 Mar;36(2):115-24. doi: 10.1016/j.jaut.2010.12.003. Epub 2011 Jan 22. PMID:21257291
Disease exacerbation of multiple sclerosis is characterized by loss of terminally differentiated autoregulatory CD8+ T cells. Cunnusamy K, Baughman EJ, Franco J, Ortega SB, Sinha S, Chaudhary P, Greenberg BM, Frohman EM, Karandikar NJ. Clin Immunol. 2014 May-Jun;152(1-2):115-26. doi: 10.1016/j.clim.2014.03.005. Epub 2014 Mar 20. PMID:24657764
Induction of regulatory T-cells from memory T-cells is perturbed during acute exacerbation of multiple sclerosis. Mohiuddin IH, Pillai V, Baughman EJ, Greenberg BM, Frohman EM, Crawford MP, Sinha S, Karandikar NJ. Clin Immunol. 2016 May;166-167:12-8. doi: 10.1016/j.clim.2016.05.001. Epub 2016 May 3. PMID:27154631